Publications in scientific journals
1. I. Zaed; Z. Rossini; F. Faedo; M. Fontanella; A. Cardia; F. Servadei: “Long-term follow-up of custom-made porous hydroxyapatite cranioplasty in adult patients: a multicenter European study. Can we trust self-reported complications?”. Journal Neurosurgical Science 2020 Sep 28 doi: 10.23736/S0390-5616.20.05138-3.2020
https://pubmed.ncbi.nlm.nih.gov/32989979/
(keyword: post market clinical follow-up)
2. Z. Rossini; A. Franzini; I. Zaed; N. Zingaretti; F. Nicolosi; B. Zanotti: “Custom-made porous hydroxyapatite cranioplasty in patients with tumor versus traumatic brain injury: a single center case series”. Journal of Word Neurosurgery. pii: S1878-8750(20)30615-X. doi: 10.1016/j.wneu.2020.03.144.2020
https://www.ncbi.nlm.nih.gov/pubmed/32272268
(keyword: case series - tumor)
3. A. Szathmari, A. Morgado, PA. Beuriat, P. Petrescu, F. DiRocco, C. Mottolese: “Cranioplasty for bone defects after craniosynostosis surgery. Case series with literature review”. Neurochirurgie, 2020 Feb 24. pii: S0028-3770(20)30031-X. doi: 10.1016/j.neuchi.2019.10.015
https://www.ncbi.nlm.nih.gov/pubmed/32105653
(keyword: pediatric case series, review - malformation)
4. B. Zanotti; A. Nataloni; R. Spaggiari; N. Zingaretti; S. Pizzolitto; PP. Parodi; F. Nicolosi; C. Morselli: “Custom-made hydroxyapatite cranioplasty: radiological and histological evidence of a bone-biomaterial osteointegration in five patients”. Asian Journal of Neurosurgery, 198-203; 2020
https://www.ncbi.nlm.nih.gov/pubmed/32181203
(keyword: osteointegration)
5. M. Ganau, H. Cebula, M. Fricia, I. Zaed; J. Todeschi ; A. Scibilia; P. Gallinaro; A. Coca; D. Chaussemy; I. Ollivier; G. Ligarotti; M. Des Neiges Santin; F. Proust; S. Chibbaro: “Surgical preference regarding different materials for custom-made allograft cranioplasty in patients with calvarial defects: Results from aninternal audit covering the last 20 years” Australian Journal of Clinical Neuroscience; 2020
https://www.ncbi.nlm.nih.gov/pubmed/32033859
(keyword: comparative studies)
6. P. Spennato; V. Canella; F. Aliberti; C. Russo; C. Ruggiero; A. Nataloni; M. Lombardo; G. Cinalli: “Hydroxyapatite ceramic implants cranioplasty in children: a restrospective evaluation of clinical outcome and osteointegration ”. Childs Nerv Syst. 2019. doi: 10.1007/s00381-019-004423-6; 2019
https://www.ncbi.nlm.nih.gov/pubmed/31786632
(keyword: case series pediatric and osteointegration)
7. C. Morselli; I. Zaed; MP. Tropeano; G. Cataletti; C. Iaccarino; Z. Rossini; F. Servadei: “Comparison between the different types of heterologous materials used in cranioplasty: a systematic review of the literature”. Journal Neurosurgical Science 2019 Oct 7. doi: 10.23736/S0390-5616.19.04779-9. [Epub ahead of print]. 2019
https://www.ncbi.nlm.nih.gov/pubmed/31599560
(keyword: adult review)
8. P.A. Beuriat; L.N Lohkamp; A. Szathmari; C. Rousselle; I. Sabatier; F. Di Rocco; C. Mottolese: “Repair of Cranial Bone Defects in Children Using Synthetic Hydroxyapatite Cranioplasty. Word Neurosurgery. 2019. 14. pii: S1878-8750(19)31326-9. doi: 10.1016/j.wneu.2019. 05.052
https://www.ncbi.nlm.nih.gov/pubmed/31100525
(keyword: case studies pediatric)
9. P. Frassanito; F. Bianchi; V. Stifano; F. Fraschetti; L. Massimi; G. Tamburini; M. Caldarelli: “Craniocerebral disproportion after decompressive craniectomy in infants: The hidden enemy of cranial repair?”. Childs Nerv Syst. 2019 May 27. doi: 10.1007/s00381-019-04166-4
https://www.ncbi.nlm.nih.gov/pubmed/31134339
(keyword: surgical technique)
10. F. Graziano; R. Maugeri; G.R. Giammalva; E. Lo Bue; G. Zabbia; D.G. Iacopino: “Pulsed radiofrquency energy device (PEAK Plasmablade™) and CustomBone® Cranioplasty: an appealing surgical rendez-vous”. British Journal of Neurosurgery [Epub ahead of print]. 2019
https://www.ncbi.nlm.nih.gov/pubmed/30856015
(keyword: surgical technique)
11. M. Klieverik; J. Miller; A. Singhal; K.S. Han; P.A. Woerdeman: “Cranioplasty after craniectomy in pediatric patients – a systematic review”. Child's Nervous System Journal Jan 4. doi: 10.1007/s00381-018-4025-1. [Epub ahead of print]. 2019
https://www.ncbi.nlm.nih.gov/pubmed/30610476
(keyword: pediatric review)
12. P. Frassanito; F. Bianchi;G. Pennisi; L. Massimi; G. Tamburini; M. Caldarelli: “The growth of the neurocranium: literature review and implications in cranial repair”. Childs Nerv Syst. 2019 Sep;35(9):1459-1465. doi: 10.1007/s00381-019-04193-1. 2019
https://www.ncbi.nlm.nih.gov/pubmed/31089851
(keyword: pediatric)
13. M. Fricia; F. Nicolosi; M. Ganau; H. Cebula; J. Todeschi; SM des Neiges; B. Nannavecchia; C. Morselli; S. Chibbaro: “Cranioplasty with porous hydroxiapatite custom-made bone flap: results from a multicentre study enrolling 149 patients over 15 years”. Journal of Word Neurosurgery. pii: S1878-8750(18)32254-X. doi: 10.1016/j.wneu.2018.09.199. [Epub ahead of print]. 2018
https://www.ncbi.nlm.nih.gov/pubmed/30315976
(keyword: case studies and complications)
14. W. Maenhoudt; G. Hallaert; JP Kafala; E. Baert; F. Dewaele; W. Bauters; D. Van Roost: “Hydroxyapatite cranioplasty: a retrospective evaluation of osteointegration in 17 cases”. Acta Neurochirurgica doi: 10.1007/s00701-018-3694-6. 2018
https://www.ncbi.nlm.nih.gov/pubmed/30276548
(keyword: osteointegration)
15. P. Frassanito; L. Massimi; G. Tamburini; F. Bianchi; A. Nataloni; V. Canella; M. Caldarelli: “Custom-made hydroxyapatite for cranial repair in a specific pediatric age group (7-13 years old): a multicenter post-marketing surveillance study”. Childs Nerv Syst. 2018 Jul 10. doi: 10.1007/s00381-018-3905-8. 2018
https://www.ncbi.nlm.nih.gov/pubmed/29987377
(keyword: surveillance, clinical studies and complications pediatric)
16. M. Still; A. Roux; M. Zanello; E. Dezamis; E. Parraga; X. Sauvageon; J.F. Meder; J. Pallud: “Independent factors affecting postoperative complication rates after custom-made porous hydroxyapatite cranioplasty: a single-center review of 109 cases”. Journal of Word Neurosurgery. pii: S1878-8750(18)30663-6. doi: 10.1016/j.wneu.2018.03.181. [Epub ahead of print]. 2018
https://www.ncbi.nlm.nih.gov/pubmed/29625304
(keyword: case series and complications)
17. B. Zanotti; N. Zingaretti; A. Verlicchi; A. Alfieri; P.C. Parodi: “Successful Strategies for Dealing with Infected, Custom-made Hydroxyapatite Cranioplasty”. Journal of Craniofacial Surgery. 2018 Mar 1. doi: 10.1097/SCS.0000000000004415. [Epub ahead of print]. 2018
https://www.ncbi.nlm.nih.gov/pubmed/29498974
(keyword: case report, complications and biomaterial characteristics)
18. A. Moles, P.M. Heudes, A. Amelot, J. Cristini, C. Salaud, V. Roualdes, T. Riem, S.A. Martin, S. Raoul, L. Terreaux, E. Bord, K. Buffenoir: “Long-Term Follow-Up Comparative Study of Hydroxyapatite and Autologous Cranioplasties: Complications, Cosmetic Results, Osseointegration”. Journal of Word Neurosurgery. pii: S1878-8750(17)32198-8. doi: 10.1016/j.wneu.2017.12.082. [Epub ahead of print]. 2018
https://www.ncbi.nlm.nih.gov/pubmed/29277595
(keyword: comparative study)
19. R. Maduri; E. Viaroli; M. Levivier; R. T. Daniel; M. Messerer: “Use of a 3D Skull Model to Improve Accuracy in Cranioplasty for Autologous Flap Resorption in a 3-Year-Old Child”. Pediatric Neurosurgery Journal. 2017;52(5):351-355. doi: 10.1159/000479329. 2017
https://www.ncbi.nlm.nih.gov/pubmed/28848112
(keyword: case report pediatric and one step)
20. D. Garcia-Gonzalez; J. Jayamohan; S.N. Sotiropoulos; S.H. Yoon; J. Cook; C.R. Siviour; A. Arias; A. Jérsusalem: “On the mechanical behavior of PEEK and HA cranial implants under impact loading”. Journal of the Mechanical Behavior of Biomedical Materials; 69:342-354. doi: 10.1016/j.jmbbm.2017.01.012. Epub. 2017
https://www.ncbi.nlm.nih.gov/pubmed/28160738
(keyword: biomaterial characteristics)
21. S. Zaccaria; S.J. Tarakan; S. Altermatt: “Hydroxyapatite ceramic implants for cranioplasty in children: a single center experience”. Child's Nervous System Journal; 33(2):343-348. doi: 10.1007/s00381-016-3327-4. 2017
https://www.ncbi.nlm.nih.gov/pubmed/28013335
(keyword: case series pediatric)
22. A Morice; F. Kolb; A. Picard; N. Kadlub; S. Puget: “Reconstruction of a large calvarial traumatic defect using a custom-made porous hydroxyapatite implant covered by a free latissimus dorsi muscle flap in an 11-year-old patient”. J. Neurosurg Pediatr. 28:1-5. [Epub ahead of print]. 2016
https://www.ncbi.nlm.nih.gov/pubmed/27791703
(keyword: case report pediatric)
23. R. Carloni; C. Herlin; B. Chaput; A. De Runz; Hersant; E. Watier; N. Bertheuil: “Scalp tissue expansion above a custom-bone hydroxyapatite cranial implant to correct sequelar alopecia on a transposition flap: a case report” World Neurosurg 2016 Sep 5. pii: S1878-8750(16)30800-2. doi: 10.1016/j.wneu.2016.08.116. 2016
http://www.ncbi.nlm.nih.gov/pubmed/27609453
(keyword: surgical tips)
24. P.A. Beuriat; A. Szathmari; B. Grassiot; F. Di Rocco; C. Mottolese: “Why a hydroxyapatite cranioplasty can be used to repair a cranial bone defect in children: Experience of 19 cases”. Neurochirurgie. 2016 Aug 17. pii: S0028-3770(16)30059-5. doi: 10.1016. 2016
http://www.ncbi.nlm.nih.gov/pubmed/27543986
(keyword: case studies pediatric)
25. B. Zanotti; N. Zingaretti; A. Verlicchi; M. Robiony; A. Alfieri; P.C. Parodi: “Cranioplasty: Review of Materials” Journal of Craniofacial Surgery. 2016
http://www.ncbi.nlm.nih.gov/pubmed/27548829
(keyword: review)
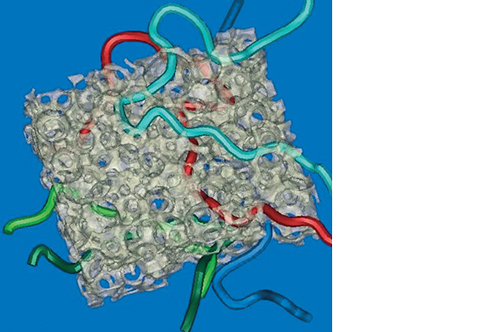
26. S. Sprio; M. Fricia; G. Maddalena; A. Nataloni; A. Tampieri: “Osteointegration in cranial bone reconstruction: a goal to achieve”. Journal of Applied Biomaterials & Functional Materials. 6:0. doi: 10.5301/jabfm.5000293. 2016
http://www.ncbi.nlm.nih.gov/pubmed/27311430
(keyword: osteointegration)
27. C. Iaccarino; PP Mattogni; B. Zanotti; S. Bellochi; A. Verlicchi; E. Viaroli; G. Pastorello; F. Sgulò; R. Ghardirpour; F. Servadei: “Septic complication following porous hydroxyapatite cranioplasty: prosthesis retention management” Journal of Neurosurgical Sciences. 2016
http://www.ncbi.nlm.nih.gov/pubmed/27175619
(keyword: case studies, complications and biomaterial characteristics)
28. A. Di Rienzo, P.P: Pangrazi; M. Riccio; R. Colasanti; I. Ghetti; M. Iacoangeli: “Skin flap complications after decompressive craniectomy and cranioplasty: proposal of classification and treatment options”. Surgical Neurology International. 7(Suppl 28):S737-S745. 2016
https://www.ncbi.nlm.nih.gov/pubmed/27904753
(keyword: case studies and complications)
29. D. Lindner; K. Schlothofer-Schumann; C. Kern; O. Marx; J. Meixensberger:: “Cranioplasty of CustomBone versus CAD based Titanium - a randomized clinical trial”. Journal of Neurosurgery Jan; 126(1):175-183. doi: 10.3171/2015.10.JNS151245. 2016
http://www.ncbi.nlm.nih.gov/pubmed/26918471
(keyword: clinical studies)
30. M. Bruneau; R. Kamouni; F. Schoovaerts; HB Pouleau; O. De Witte: “Simultaneous Image-Guided Skull Bone Tumor Resection and Reconstruction With a Preconstructed Prosthesis Based on an OsiriX Virtual Resection”. Neurosurgery. 2015
http://www.ncbi.nlm.nih.gov/pubmed/26287551
(keyword: surgical technique - one step)
31. C. Iaccarino; E. Viaroli; M. Fricia; E. Serchi; T. Poli; F. Servadei: “Preliminary results of a prospective study on methods of cranial reconstruction”. Journal of Oral and Maxillofacial Surgery. S0278-2391(15)01007-1.doi: 10.1016/j.joms.2015.07.008. 2015
http://www.ncbi.nlm.nih.gov/pubmed/26253012
(keyword: clinical studies)
32. R. Carloni; B. Hersant; R. Bosc; C. Le Guerinel; J.P. Meningaud: “Soft Tissue Expansion and Cranioplasty: For Which Indications?” Journal of Cranio-Maxillofacial Surgery, pii: S1010-5182(15)00191-2.doi:10.1016/j.jcms. 2015
http://www.ncbi.nlm.nih.gov/pubmed/26189146
(keyword: surgical tips)
33. M. Fricia; M. Passanisi; F. Salamanna; A. Parrilli; G. Giavaresi; M. Fini: “Osteointegration in custom-made porous hydroxyapatite implants: from reconstructive surgery to regenerative medicine”. World Neurosurg. 2015 Mar 25. pii: S1878-8750(15)00294-6. doi: 10.1016/j.wneu. 2015.03.027. 2015
http://www.ncbi.nlm.nih.gov/pubmed/25819529
(keyword: osteointegration)
34. B. Zanotti; A.Verlicchi; R. Stefini; A.C. Salgarelli; N. Zingaretti; P.C. Parodi; M. Casadei; M. Robiony: “Surgical pitfalls with custom-made porous hydroxyapatite cranial implants” Plastic and Aesthetic Research (journal of Asia-Pacific Association of Medical Research and European Residents in Plastic Surgery), Vol. 2, Issue 1, IP: 95.227.84.84. 2015
(keyword: surgical tips)
35. B. Zanotti; A.Verlicchi; S. Indiani; S.A. Scarparo; N. Zingaretti; P.C. Parodi: “Spontaneous fractures in custom-made porous hydroxyapatite cranioplasty implants: is fragility the only culprit?” Acta Neurochirurgica ;157(3):517-23. doi: 10.1007/s00701-014-2319-y. 2015
http://www.ncbi.nlm.nih.gov/pubmed/25588747
(keyword: biomaterial characteristics)
36. M. Fricia; M. Passanisi: “Long-term results following porous hydroxyapatite bilateral cranioplasty: an 8-year radiological follow-up”. Progress in Neuroscience, Vol. 2 N.1-4. 2014
http://www.progressneuroscience.com/index/vol_3,_n_1-4,_2015.htm
(keyword: long-term follow-up)
37. B. Zanotti, N. Zingaretti; D. Almesberger; A. Verlicchi; R. Stefini; M. Ragonese; G.F. Guarnieri; P.C. Parodi: “Enhancing dermal and bone regeneration in calvarial defect surgery”. Indian Journal of Plastic Surgery. 47(3):325-32. doi: 10.4103/0970-0358.146581, Vol. 47 Issue 3. 2014
http://www.ncbi.nlm.nih.gov/pubmed/25593416
(keyword: bone regeneration cranioplasty, osteointegration)
38. R.Stefini; B. Zanotti; A.Nataloni; R.Martinetti; M.Scafuto; M.Colasurdo; A. Tampieri: “The efficacy of custom made porous hydroxyapatite devices for cranioplasty: evaluation of Post-Marketing data on 2697 patients” Journal of Applied Biomaterials & Functional Materials, 13(2): e136 - e144. 2014
http://www.ncbi.nlm.nih.gov/pubmed/25589160
(keyword: biomaterial characteristics)
39. F. Servadei, C. Iaccarino: “Perspective: The therapeutic cranioplasty still needs an ideal material and surgical timing”. World Neurosurgical. pii: S1878-8750(14)00752-9. doi: 10.1016/j.wneu.2014.08.031. 2014
http://www.ncbi.nlm.nih.gov/pubmed/25153284
(keyword: review)
40. P. Frassanito; G. Tamburini; L. Massimi; C. Di Rocco; A. Nataloni; G. Fabbri; M. Caldarelli: “Post-marketing surveillance of CustomBone Service implanted in children under 7 years hold”. Acta Neurochirurgica. 157(1):115-21. doi: 10.1007/s00701-014-2254-y. 2014
http://www.ncbi.nlm.nih.gov/pubmed/25326712
keyword: case studies and complications pediatric)
41. A. Di Rienzo, M. Iacoangeli, L. Alvaro, R. Colasanti, M. Dobran, LG Di Somma, E. Moriconi, A. Scerrati: “The sinking bone syndrome?”. Neurologica medico-chirurgica Journal (The Japan Neurosurgical Society), 53(5):329-35. 2013
http://www.ncbi.nlm.nih.gov/pubmed/23708225
(keyword: surgical technique)
42. J.-M. Lemée, D. Petit, M. Splingard, P. Menei: “Autologous bone flap versus hydroxyapatite prosthesis in first intention in secondary cranioplasty after decompressive craniectomy: A French medico-economical study”. Journal de Neurochirurgie. 10.138. 2013
http://www.ncbi.nlm.nih.gov/pubmed/23414773
(keyword: comparison other material)
43. R. Stefini, G. Esposito, B. Zanotti, C. Iaccarino, M. Fontanella, F. Servadei: “Use of custom made porous hydroxyapatite implants for cranioplasty: post-operative analysis of complications in 1549 patients”. Surgical Neurology International. Vol 4 / ISSUE 1. 2013
http://www.ncbi.nlm.nih.gov/pubmed/23493459
(keyword: case studies and complications)
44. P. Frassanito, P. De Bonis, PP Mattogno, A. Mangiola, M. Novello, D. Brinchi, A. Pompucci, C, Anile: “The fate of a macroporous hydroxyapatite cranioplasty four years after implantation: macroscopical and microscopical findings in a case of recurrent atypical meningioma”. Clin Neurol Neurosurg. Dec 26. pii: S0303-8467(12)00610-5. 2012
http://www.ncbi.nlm.nih.gov/pubmed/23273380
(keyword: osteointegration)
45. A. Di Rienzo, M. Iacoangeli, LG Di Somma, L. Alvaro, N. Nocchi, A. Scerrati: “Shape modifications of porous hydroxyapatite prostheses to improve rigid implant fixation: Experience in 12 cases”. Surgical Neurology International. 3:161. 2012
http://www.ncbi.nlm.nih.gov/pubmed/23372977
(keyword: case studies)
46. A.T. Adetchessi; G. Pech-Gourg; P. Metellus; S. Fuentes: “Fracture précoce d’une cranioplastie en céramique macropoereuse d’hydroxyapatite”. Journal de Neurochirurgie. Dec; 58(6):382-5. 2012
http://www.ncbi.nlm.nih.gov/pubmed/22898300
(keyword: case report)
47. P. De Bonis; P. Frassanito; A. Mangiola; C. Ginevra Nucci; C. Anile and A. Pompucci : “Cranial repair: how complicated is filling a hole?”. Journal of neurotrauma n° 29, 1071-1076. 2012
http://www.ncbi.nlm.nih.gov/pubmed/22648192
(keyword: surgical technique)
48. L.A. Wehrli, N. Zweifel N, R. Weil, S. Altermatt: “Juvenile Psammomatoid Ossifying Fibroma of the Forehead, Radical Resection, and Defect Coverage with a Hydroxyl-Apatite Composite-A Case Report”. European Journal of Pediatric Surgery. 2012
http://www.ncbi.nlm.nih.gov/pubmed/22648192
(keyword: case report pediatric – one step)
49. H. Hardy; E. Tollard; S. Derreya; P. Delcampe; J. Péron; P. Fréger; F. Proust: “Tolérance clinique et degré d’ossification des cranioplasties en hydroxyapatite de larges défects osseux : Clinical and ossification outcome of custom-made hydroxyapatite prothese for large skull defect”. Journal de Neurochirurgie n° 58, 25-29. 2012
http://www.ncbi.nlm.nih.gov/pubmed/22030170
(keyword: clinical studies and osteointegration)
50. L. Martini; G. Staffa; G. Giavaresi; F. Salamanna; A. Parilli; E. Serchi; D. Pressato; E. Arcangeli; M. Fini: “Long-term results following a cranial hydroxyapatite prosthesis implantation in a large skull defect model”. Journal of Plastic and Reconstructive Surgery, 625-635. 2012
http://www.ncbi.nlm.nih.gov/pubmed/22183498
(keyword: osteointegration)
51. G. Staffa; A. Barbanera; A. Faiola; M. Fricia; P. Limoni; R. Mottaran; B. Zanotti; R. Stefini: “Custom made bioceramic implants in complex and large cranial reconstruction: a two-year follow-up” Journal of Cranio-Maxillofacial Surgery, 65-70. 2012
http://www.ncbi.nlm.nih.gov/pubmed/21640597
(keyword: clinical studies)
52. B. Zanotti; A. Verlicchi; M. Robiony; P.C. Parodi: “Surgical calvarial demolition and reconstruction: procedure, implants and results”, Topics in Medicine Journal, Vol. 16. 2011
(keyword: surgical technique - one step)
53. C. Iaccarino; V. Ramponi; R. Ghardirpour; F. Carinci; F. Servadei: “Porous hydroxyapatite custom made cranioplasty: the 3d design techniques prostheses in 21 patients”. Journal of Osteology and Biomaterials, vol. 2, p. 43-53, ISSN: 2036-6795. 2011
(keyword: case studies)
54. G. Messina; I. Dones; A. Nataloni; A. Franzini: “Histologically demonstrated skull bone integration in a hydroxyapatite prosthesis in a human”. Acta Neurochirurgica, PMID 21491191, 1-2. 2011
http://www.ncbi.nlm.nih.gov/pubmed/21491191
(keyword: case report osteointegration)
55. E. Rampino Cordaro; S. Calabrese; G.P. Faini; B. Zanotti; A. Verlicchi; P.C. Parodi: “A method to thicken the scalp in calvarian reconstruction”. The Journal of Cranial Surgery, Vol. 22, 598-601. 2011
http://www.ncbi.nlm.nih.gov/pubmed/21403566
(keyword: surgical technique)
56. P. De Bonis; A. Pompucci; A. Mangiola; L. Rigante; C.Anile: “Post-traumatic hydrocephalus after decompressive craniectomy: an underestimated risk factor”. Journal of neurotrauma n° 27, 18-24. 2010
http://www.ncbi.nlm.nih.gov/pubmed/20812777
(keyword: surgical technique)
57. A. Della Pupa; R. Mottaran; R. Scienza: “Image-guided cranial osteoma resection and bioceramic porous hydroxyapatite custom-made reconstruction in a one-step surgical procedure. Technical notes and illustrative case”. Acta Neurochirurgia n° 152, 155-159. 2010
http://www.ncbi.nlm.nih.gov/pubmed/19430722
(keyword: case report tumor – one step)
58. G. Staffa; A Nataloni; G. Compagnone; F. Servadei: “Custom made cranioplasty prostheses in porous hyoxyapatite using 3D design techniques: 7 years’ experience in 25 patients”. Acta Neurochirurgia n° 149, 161-170. 2007
http://www.ncbi.nlm.nih.gov/pubmed/17242849
(keyword: case studies)
*Please note that outside of the US, the product is referred to as CustomBone Service. In the US the name for the device is CustomizedBone Service. These referenced articles may refer to the device as CustomBone Service, rather than CustomizedBone Service, however, the devices are the same. Also please note that in the US, the device is indicated for patients above 7 years of age.